Summary:
How frequently do you experience pain or tenderness around your jaw? If so, it could be a major indicator of a TMJ disorder.
TMJ, or Temporomandibular Joint disorder, causes pain and discomfort in and around the jaws, muscles, and ligaments. The leading causes of this disorder are usually teeth grinding, jaw injuries, and arthritis.

If your TMJ disorder is frequent and recurring, you should consider visiting a West Columbia dentist who can address your issue and suggest effective treatment plans. These professionals help ease your pain and enhance your mandible movement.
However, a majority of people have limited or no idea about treating TMJ disorder. Many people ignore it, mistaking it for normal pain.
Keeping this in mind, we shall walk you through critical topics like:
- Understanding TMJ Disorder
- Different Types of TMJ Disorders – Explained!
- Procedure for Diagnosing TMJ Disorder
- Treatment Solutions For Addressing TMJ Disorder
Continue reading as we explore TMJ disorder and its treatment plan in the following sections.
Understanding TMJ Disorder
Do you often experience pain and stiffness around your jaw joints that restricts your ability to speak, chew, or even smile?
Relax; you are not the only one going through this. Stats suggest that over 31% of the population experience these symptoms, which signifies that they have jawbone disorder.
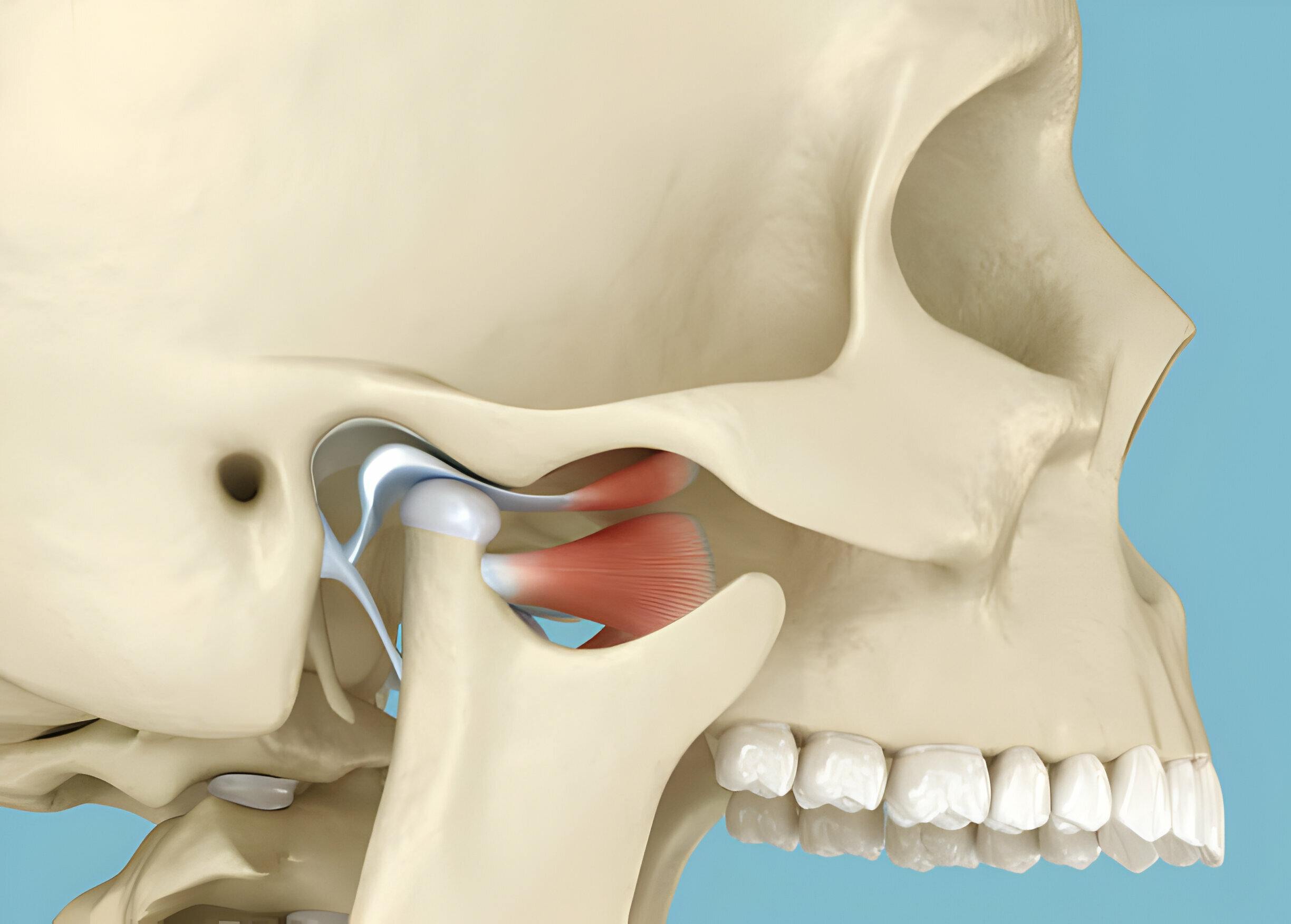
The TMJ joint (or Temporomandibular Joint) connects your jawbone to your skull, enabling you to move your jaw joints and muscles to move freely. People with TMJ disorder experience symptoms like pain, tenderness, stiffness, and popping or clicking sounds when they move their jaw while opening their mouth or chewing. Others may also experience ear aches or headaches.
What Causes TMJ?
Multiple factors can contribute to jawbone disorder, including bruxism or teeth grinding, malocclusion, mandible injuries, clenching, and arthritis. During such times, it’s best to connect with your nearest dentist for jawbone disorder, which can elevate your condition and enhance your quality of life.
Different Types Of TMJ Disorders – Explained!
The jawbone facilitates mandible movement, enabling essential functions such as speaking, chewing, and swallowing. However, when it escalates to temporomandibular joint disorder, it can lead to a range of discomforts and complications.
Here are the different types of disorders that you need to know:
Myofascial Pain Syndrome (MPS)
Myofascial pain syndrome is the most prevalent type of jawbone disorder, characterized by discomfort or pain in the muscles responsible for mandible movement.
This condition often manifests as muscle tenderness, restricted jaw movement, and aching facial pain. Due to the persistent discomfort, patients may experience difficulty performing everyday tasks such as chewing or speaking.
Internal Derangement
Internal derangement involves structural abnormalities within the TMJ, typically affecting the positioning of the disc or cushion that acts as a buffer between the jawbone and the skull.
Displacement or dislocation of this disc can result in clicking, popping, or grating noises during mandible movement, along with episodes of jaw locking or limited range of motion.
Degenerative Joint Disease (Osteoarthritis)
Degenerative joint disease, commonly called osteoarthritis, occurs when the cartilage within the TMJ gradually deteriorates over time. This degeneration leads to inflammation, stiffness, and pain in the affected joint, particularly in older individuals.
Osteoarthritis-related jawbone disorder can significantly impair function and may necessitate ongoing management to alleviate symptoms and preserve joint function.
Bruxism-related Disorder
Bruxism, characterized by involuntary teeth grinding and clenching, represents a common contributing factor to jawbone disorders. Chronic bruxism places excessive stress on the TMJ and associated muscles, leading to muscle fatigue, joint inflammation, and dental complications such as enamel wear or tooth fractures. Individuals who grind their teeth may experience pain, headaches, and jawbone disorder.
Procedure for Diagnosing Disorder
Diagnosing TMJ disorder involves a multi-step approach to understand the patient’s symptoms of TMJ and assess the function of the joint.
Here’s an outlook on the diagnostic process:
Step 1 – Medical History Assessment
A specialist dentist initiates the diagnosis by discussing the patient’s medical history, focusing on symptoms related to jaw pain, clicking sounds, chewing difficulties, and any prior injuries or treatments.
Step 2 – Physical Examination
Once your medical history is assessed, a dentist thoroughly examines the joint and surrounding muscles. It includes assessing the joint for tenderness, evaluating the jaw’s range of motion, and observing any signs of TMJ and mandible misalignment.
Step 3 – Diagnostic Imaging
TMJ professionals may sometimes recommend diagnostic imaging such as X-rays, CT scans, or MRI to obtain detailed images of the jawbone and surrounding structures. These images help identify any structural abnormalities or joint disorders.
Step 4 – Functional Assessment
Dentists also perform functional tests to evaluate the jaw’s movement during various activities, such as opening and closing the mouth, chewing, and speaking. These tests provide valuable insights into the jawbone’s function and help identify abnormalities in mandible movement.
Treatment Solutions For Addressing Jawbone Disorder
The complex nature of TMJ disorders and their potential impact on daily activities makes it crucial to adopt a holistic approach to address the condition.
Here are some TMJ therapy solutions that help in the management of jawbone disorders:
-
Lifestyle Modifications
Patients should make lifestyle adjustments for TMJ treatment in Columbia, SC. This involves techniques like stress and tension release, as stress-related habits like teeth clenching or grinding can cause TMJ discomfort. Additionally, dietary modifications such as avoiding hard or chewy foods can help reduce mandible strain and promote healing.
-
Custom Oral Appliances
For individuals experiencing nocturnal bruxism (teeth grinding) or clenching, custom-fitted oral appliances such as splints or night guards can help protect the teeth and mitigate jawbone-related pain and discomfort. These appliances stabilize the jaw joint, distribute bite forces evenly, and prevent further damage to the temporomandibular joint and surrounding structures.

-
Orthodontic Interventions
Malocclusion (misalignment of the teeth) and bite discrepancies can contribute to jawbone dysfunction by placing undue stress on the jaw joint. In such cases, orthodontic treatment modalities may be recommended to correct alignment issues and improve occlusal harmony including braces, clear aligners, or other orthodontic appliances.
-
Surgical Interventions
Surgical procedures such as arthrocentesis (joint lavage), arthroscopy, or open joint surgery may be indicated to address underlying anatomical issues, repair damaged joint structures, or replace irreversibly damaged dental TMJ components. Before considering surgical intervention, a thorough evaluation by a qualified surgeon is essential to assess preparedness and discuss potential risks and benefits.
Takeaway
- TMJ disorder is associated with symptoms like jaw pain, tenderness, stiffness, and clicking sounds, along with possible ear aches or headaches.
- Jawbone disorders can result from various factors, such as teeth grinding (bruxism), mandible injuries, malocclusion, clenching, and arthritis.
- Diagnosing jawbone disorder involves multiple steps, including a thorough medical history assessment, physical examination, diagnostic imaging, and functional assessment of mandible movement.
- Lifestyle changes, such as stress reduction techniques and dietary adjustments, can significantly help manage jawbone symptoms by reducing mandible strain and promoting healing.
- Customized oral appliances like splints or night guards can safeguard teeth from nighttime bruxism and aid in stabilizing the mandible joint, evenly distributing bite forces to prevent further damage.
- Are you experiencing similar jaw pain but confused about what it is? Talk to our Carolina Smiles Family Dentistry experts today!

